Background
Genomic abnormalities such as del(17p)/TP53 mutation, del(11q), and unmutated IGHV are risk factors that predict inferior outcomes with chemoimmunotherapy (CIT) in patients (pts) with CLL/SLL (Byrd J Clin Oncol 2006). Mutations in BIRC3, NOTCH1, SF3B1, and XPO1 have also been associated with poor outcomes with CIT in pts with CLL (Foa Haematologica 2013; Jain Am J Hematol 2016). Ibrutinib (ibr) is the only once-daily Bruton's tyrosine kinase inhibitor with significant progression-free survival (PFS) and overall survival (OS) benefit shown in multiple randomized phase 3 studies versus established therapies in pts with previously untreated or relapsed/refractory CLL/SLL. Superior outcomes were demonstrated with ibr-based therapy versus comparators in the overall population, and in pts with high-risk disease features, such as TP53 aberrations, del(11q), and/or unmutated IGHV in the RESONATE-2 study of first-line single-agent ibr (Burger Leukemia 2020) and in the iLLUMINATE study of first-line ibr-obinutuzumab (Moreno Lancet Oncol 2019). In pts with relapsed/refractory CLL/SLL who were treated with ibr, mutations in BIRC3, NOTCH1, SF3B1, or XPO1 had no significant impact on the PFS benefit conferred by ibr (Byrd Blood 2019). To better understand outcomes in pts with previously untreated CLL with various high-risk genomic features, including integrated FISH cytogenetics and single gene mutations, we performed a pooled analysis of two phase 3 studies of ibr-based therapy in the first-line treatment of CLL/SLL (RESONATE-2 and iLLUMINATE).
Methods
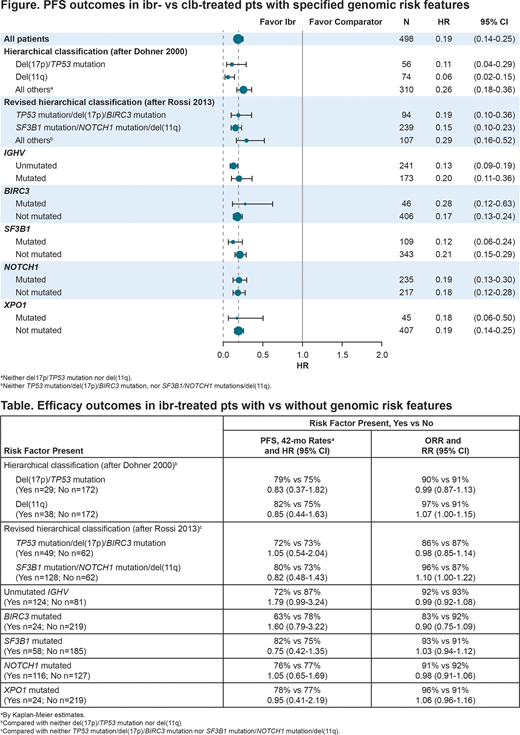
In RESONATE-2 (NCT01722487), pts aged ≥65 years without del(17p) were randomized to single-agent ibr or chlorambucil (clb). In iLLUMINATE (NCT02264574), pts aged ≥65 years, or <65 years with coexisting conditions or del(17p)/TP53 mutation, were randomized to ibr-obinutuzumab or clb-obinutuzumab. A central lab performed FISH or targeted next generation sequencing, respectively, to examine for del(17p) and del(11q), or mutations in IGHV, TP53,BIRC3, SF3B1, NOTCH1, or XPO1. Clinical outcomes (PFS and overall response rate [ORR]) were determined for subsets defined by FISH cytogenetics or single gene mutations alone or in combination (Dohner N Engl J Med 2000; Rossi Blood 2013). PFS (reported as 42-mo Kaplan-Meier estimates and hazard ratios [HRs]), ORR (with rate ratios), and safety were compared between (1) ibr- versus clb-based therapies and (2) ibr-treated pts with vs without high-risk genomic CLL features.
Results
The pooled analysis included 498 pts treated with first-line ibr-based or clb-based therapy (n=249 each) with median follow-up of 49.1 mos (range, 0.1-78.7). Ibr-based therapy significantly improved ORR and PFS vs comparator (clb-based) therapy. At 42 mo, PFS rates were significantly higher across high-risk genomic subgroups in ibr-treated pts (63-82%) compared with clb-treated pts (6-34%), and consistent PFS benefit with ibr was observed across all high-risk genomic subgroups (Figure). When comparing ibr-treated pts with specified high-risk genomic features vs those without, PFS and ORR were comparable in the different subgroups, including pts with unmutated vs mutated IGHV (PFS HR, 1.79, 95% CI 0.99-3.24) or mutated vs not mutated NOTCH1 (PFS HR, 1.05, 95% CI 0.65-1.69) (Table). Improved outcome was also noted for pts with del(17p)/TP53 mutated/BIRC3 mutated, the highest risk category per Rossi 2013 (HR 1.05, 95% CI 0.54-2.04). At a median duration of ibr treatment of 35.7-43.8 mo across these high-risk subgroups, there were no meaningful differences in the rates of treatment-emergent adverse events (AEs) of any grade or grade ≥3 AEs compared to those of the overall population.
Conclusions
This integrated analysis of pts undergoing first-line ibr-based treatment, with up to 79 mo follow up, demonstrated similar PFS and ORR for ibr-treated pts with or without high-risk genomic features, and confirmed significant PFS and ORR benefits with ibr-based therapy versus clb (± obinutuzumab). This analysis across two phase 3 studies demonstrated the efficacy of first-line ibr-based treatment irrespective of cytogenetic and mutational risk features, including those with unmutated IGHV, NOTCH1 mutation, and those with the highest risk classification of del(17p)/TP53 mutation/BIRC3 mutation.
Burger:Gilead, Janssen, Novartis, TG Therapeutics, and Pharmacyclics LLC, an AbbVie Company: Other: Travel/accomodations/expenses, Speakers Bureau; Janssen: Consultancy, Honoraria, Research Funding; BeiGene, Gilead, TG Therapeutics, and Pharmacyclics LLC, an AbbVie Company: Research Funding. Robak:BioGene: Honoraria, Research Funding; UCB: Honoraria, Research Funding; UTX-TGR: Research Funding; Bristol Meyers Squibb: Research Funding; Momenta: Consultancy; Medical University of Lodz: Current Employment; Pharmacyclics LLC, an AbbVie Company: Honoraria, Research Funding; AstraZeneca: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company), Research Funding; Takeda: Consultancy; Sandoz: Consultancy, Honoraria; Octapharma: Honoraria; Pfizer: Research Funding; GSK: Research Funding; Roche: Consultancy, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company), Research Funding; Acerta: Research Funding; Morphosys: Research Funding; Janssen: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company), Research Funding. Demirkan:AbbVie, Amgen, AstraZeneca, and Roche: Consultancy; AbbVie, AstraZeneca, Janssen, and Pharmacyclics LLC, an AbbVie Company: Research Funding; AbbVie, Amgen, and Janssen: Speakers Bureau; AbbVie, Amgen, Janssen, and Pfizer: Other: Travel/accommodations/expenses. Bairey:AbbVie: Consultancy; Janssen: Consultancy, Research Funding. Moreno:Janssen: Speakers Bureau; AbbVie and Janssen: Research Funding; Janssen, AbbVie, Sunesis, and AstraZeneca: Consultancy. Simpson:BeiGene: Current Employment, Current equity holder in publicly-traded company; AbbVie and Janssen: Honoraria, Other: Travel/accommodations/expenses; AbbVie, Acerta, Amgen, BeiGene, Celgene, GlaxoSmithKline, Janssen, Merck Sharp & Dohme, Roche, Sanofi, and Pharmacyclics LLC, an AbbVie Company: Research Funding. Munir:F. Hoffmann-La Roche: Consultancy, Other: Medical writing support, furnished by Scott Battle, PhD, of Health Interactions, was funded by F. Hoffmann-La Roche Ltd, Basel, Switzerland; Alexion: Honoraria. Stevens:Amgen, MorphoSys: Consultancy. Dai:Pharmacyclics LLC, an AbbVie Company: Current Employment; AbbVie, Bristol-Myers Squibb, Exelixis, Gilead, GlaxoSmithKline, and Revance: Current equity holder in publicly-traded company. Cheung:Pharmacyclics LLC, an AbbVie Company: Current Employment, Patents & Royalties: and other intellectual property; AbbVie and Eli Lilly: Current equity holder in publicly-traded company. Kwei:Pharmacyclics LLC, an AbbVie Company: Current Employment; AbbVie and Gilead: Current equity holder in publicly-traded company. Lal:Pharmacyclics LLC, an AbbVie Company: Current Employment; The Permanente Medical Group (spouse): Current Employment; AbbVie, Clovis, Gilead Sciences, Infinity, Reviva Pharmaceuticals, and The Permanente Medical Group: Current equity holder in publicly-traded company. Hsu:Pharmacyclics LLC, an AbbVie Company: Current Employment; AbbVie: Current equity holder in publicly-traded company. Kipps:AbbVie, Genentech-Roche, Oncternal, and Pharmacyclics LLC, an AbbVie Company: Research Funding; AbbVie, Celgene, Genentech-Roche, Gilead, and Pharmacyclics LLC, an AbbVie Company: Consultancy. Tedeschi:AstraZeneca: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen spa: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Department of Hematology Niguarda Hospital Milano: Current Employment; Sunesis: Consultancy; AbbVie: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BeiGene: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal